The pandemic time has unveiled a plethora of opportunities and brought in a paradigm shift in work culture – Remote Working, driven by technology. This has enabled the continuation of services irrespective of location and time without compromising the quality-of-service delivery. But this remote working is not a new concept in Radiology. Many radiologists have been supporting the clinicians irrespective of their location and time through teleradiology and delivering quality patient care without delay.
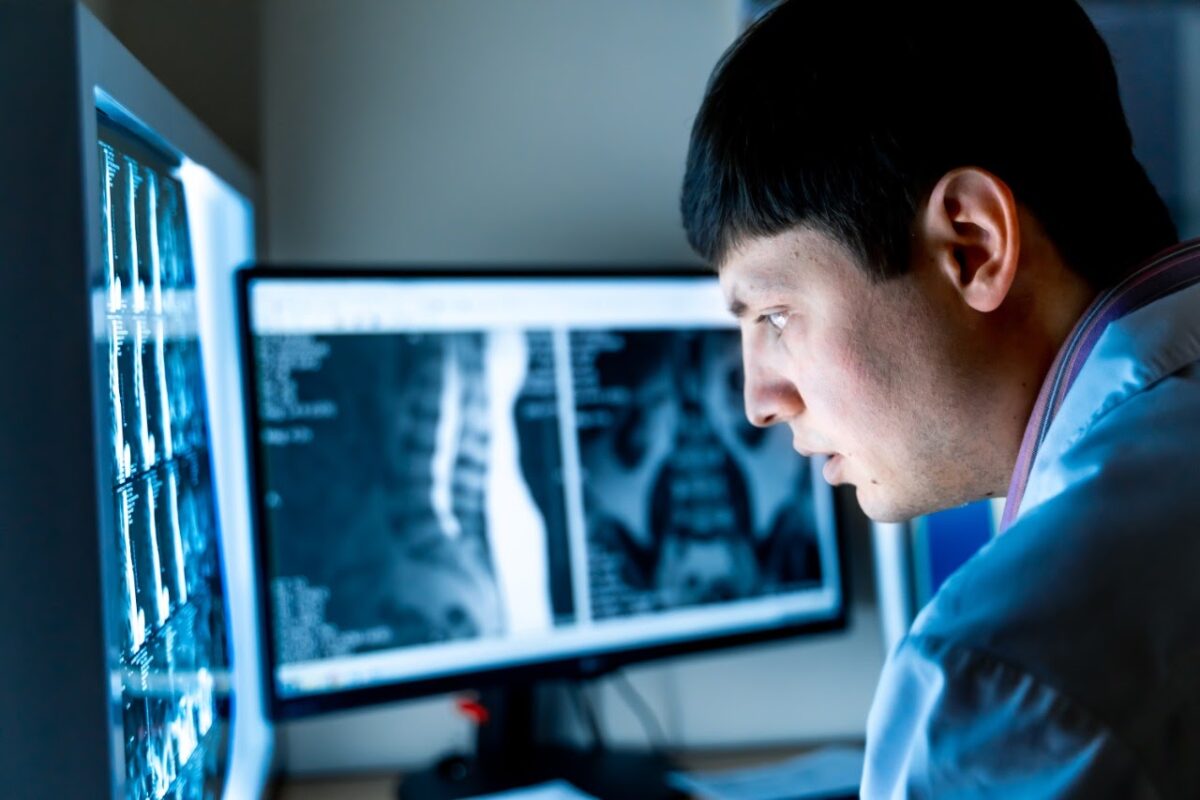
Teleradiology, identified with remote working is actually vibrant, spontaneous, and into real-time work. All this is possible because of PACS.
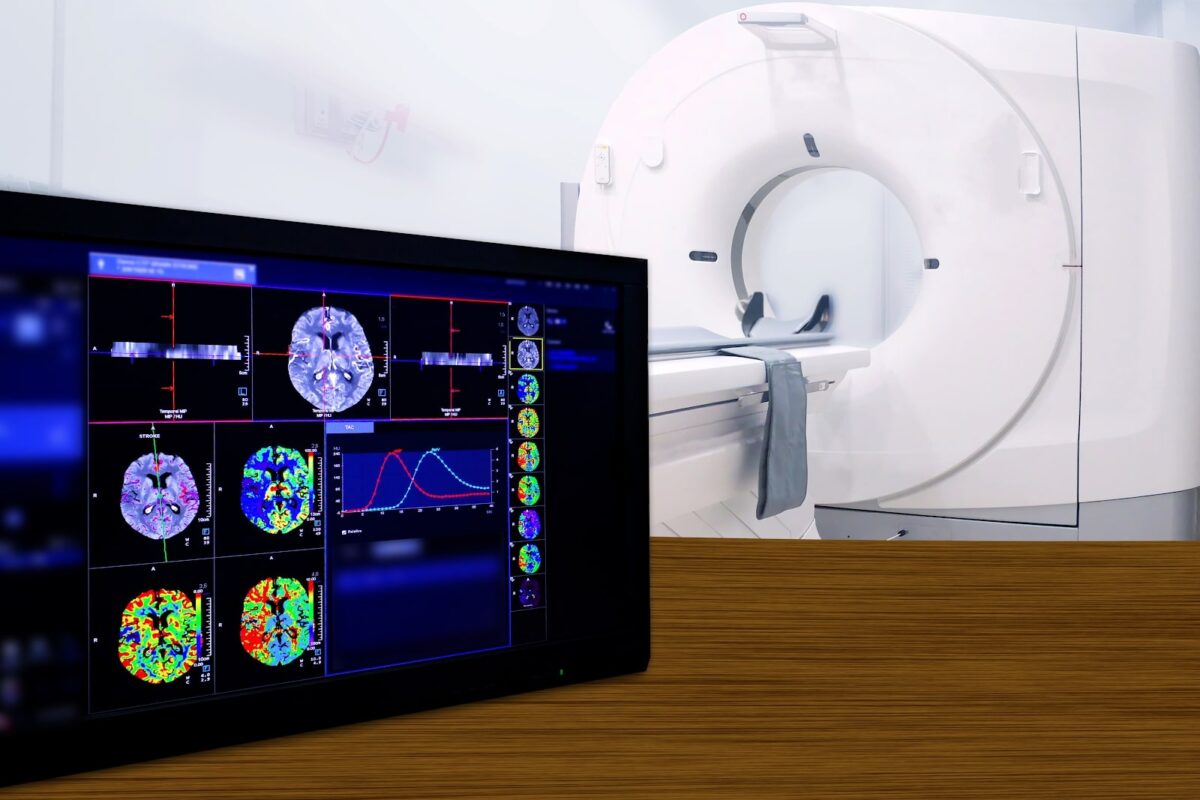
PACS – Picture Archiving and Communication System; a system involved in acquiring the medical images, transmission, viewing, storage, and retrieval of same images. Basically, PACS is an electronic version of the file room and reading room for radiologists. PACS works as a host that integrates the radiological images acquired from different radiological imaging modalities (X-Ray, Ultrasound, CT, MRI, PET Scan, Nuclear Medicine, etc…) with a network of information system (RIS and or HIS), EMR, different work stations and image storage/archival system.
Since 1980, PACS has undergone many transformations in multiple ways. All these have been worked out to improve – the transmission of images without any compromise on its quality, archiving and retrieving of data (images and other information) for reference without any delay, communication between the referring Physician, and reporting radiologist. The fundamental parts of PACS are – imaging acquisition, display workstations, archive servers. The workflow is customized based on the modality of images and criticality of the cases marked in the raised work orders

Today, the Web-based PACS offers many additional features like AI-Assisted Decision Support systems, Multi-Media Enhanced Reporting (MMER), an intuitive user interface, intelligent work aids (personalized tools and layout), mobile extensions, multimedia communication tools, etc that boost reading/reporting, making it a smart PACS. It is a coordinator between multiple processes (software & hardware) and applications enabling the image reporting as a real-time service supporting referring physicians.
The benefit of all these features has resulted in reduced TAT, improved productivity of department, better management of emergency / critical cases, and maintenance of data security. It also enables the viewing of images for reporting from anywhere – inside the department or at the nursing station or on mobile gadgets (mobile/notepads/laptops) or remote reporting sites (Teleradiology).
PACS infrastructure is evolving with advancements in medical imaging technologies and it is highly scalable to keep up the pace with the increasing number of imaging and reporting. This scalability can involve – the addition of more no. of imaging modalities, storage space, no. of work stations, integration of artificial intelligence and machine learning or any other features.
PACS in Hospitals / Tele-reporting service providers with different modalities and multiple work stations use Vendor Neutral Archive (VNA) which brings about compatibility between the different software of imaging machines and PACS’ networking. VNA ensures seamless functioning of data receiving, transmission, integration, and archival and saves time by providing one viewing experience/interface irrespective of the origin of data acquisition.

Cloudex Solutions: extending teleradiology with cloud-based PACS
Cloudex has set its tele-reporting infrastructure with the advanced smart PACS that provides a convenient workflow and easy-to-use interfaces/dashboard. These advanced online PACS is capable of handling multiple modalities and multiple workstations providing the browser as the main viewing tool enhancing the faster TAT.
The teleradiologists login into the browser and start with the flexibility of time ensuring the tele-reporting services for 24x 7 x 365. Now hospitals / diagnostic centers have the advantage of need-based tele-reporting depending on the imaging modality/subspecialty/timing (full time or night hawk services) instead of traditional reporting apart without a huge investment in digitalized workflow and storage. The experience of the PACS administrator adds a lot of value especially in critically marked/emergency cases apart from their regular maintaining or managing or troubleshooting roles.
Cloudex with its flexibility in working and range of tele-reporting services aims to support its clients (healthcare service providers) in overcoming obstacles faced while delivering patient care and have a winning edge towards patient satisfaction.
At Cloudex, we support you to have that winning edge.