Once upon a time, teleradiology was considered as a fragmented and interrupted experience where the images, texts, and speeches were getting delivered on a different medium. And the poor communication between the referring physician and teleradiologist might have resulted in confusion in the patient’s mind or the high cost or undesirable clinical outcomes.
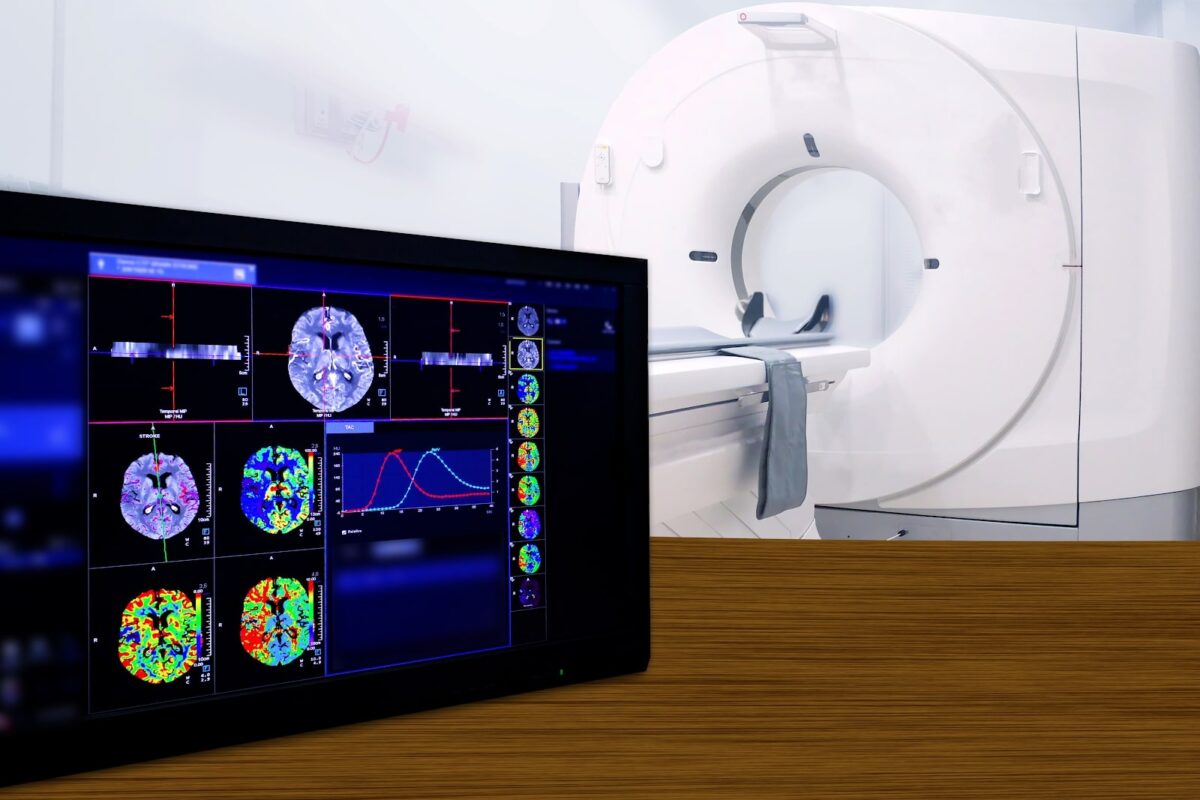
Currently, technological advances have revolutionized the way teleradiology is conducted and are contributing to quality healthcare service delivery. Today, teleradiology represents the integration of the many advanced multimedia technologies which supports the upload/download of reports along with other necessary support documents (other than radiological images), display of images (multiple viewing/screening options), tools for image annotation, image/report archival and retrieval, communication between the group/team, audio reporting and its conversion into text report are some of the important features facilitating the remote reporting equivalent to real-time reporting.
At present, Teleradiology addresses the key concern of the referring physician – accurate report at the earliest with the provision of communicating with teleradiologists in real-time.
These concerns get addressed and benefit him in multiple ways.
- Benefit of Support from the extended team during the deciding moments becomes crucial for those who are based in healthcare centers where the radiology department works in stipulated working hours or patients are referred to other centers for radiology services. In such a scenario, the treating physician is benefitted by receiving accurate reports within the decided TAT and can interact with the teleradiologist for further clarification. Overall, the referring physician has an extended team outside his team (employed/assigned team) to support him in providing quality patient care and on whom he can rely during his crucial deciding moments.
- Benefit of 24 x 7 Reporting services empowers the referring physician in providing quality patient care round the clock without any delay. This benefits the physician as well as the patient in saving the time and cost, the shift of patient to emergency service and unexpected situation.
- Benefit of Expert Opinion when an ambiguous situation. A qualified and expert panel of subspecialists can support the referring physician in more than one way – correct diagnosis, prognosis, and working out the appropriate treatment plan or in understanding/monitoring the treatment outcome. This works wonders for the multispecialty hospitals who need the subspecialty reporting and expert opinions for critical cases additional to their regular radiologist’s reporting; especially in cases of Orthopaedic, Neurology, Oncology, Paediatric or Emergency to name a few.
- Benefit of Remote Reporting has brought about a paradigm shift in the quality of patient care extended in primary or secondary care centers located in tier 2 / 3 towns or geographically challenging locations. Teleradiology has built a connection where referring physicians can interact with the reporting teleradiologist in real-time. As a result, Referring Physician can inform the patient about the criticality of the patient in emergency cases and guide the patient in taking appropriate action or referring a patient to comprehensive healthcare centers at right time.
- Benefit of Selective Reporting services is an option where the referring physician can choose from different types of teleporting services based on the need; like during the absence of regular radiologists due to holiday/weekend / off-duty / night-time. The different services available to opt for are night call reporting, weekend reporting, overload reporting, vacation reporting. All these selective options are available to ensure patient care without any delay.
- Benefit of Answers to the queries of Patient which helps in building trust. Many times, the internet-savvy patient from the metro and tier 1 town throws a series of queries for a better understanding of the situation and for taking appropriate action (shift to a specialty center for surgery/treatment). The patient’s interaction with the reporting teleradiologist who has given the detailed imaging report helps in briefing those critical characteristics playing a crucial role in prognosis. The building of trust depends on many aspects and this can prove to be one of the ways.
Cloudex Radiology Solutions empowers the Referring Physician with a winning edge…
Cloudex teleradiology services empowered with its qualified & experienced experts and subspecialty teleradiologist extends the benefits of technologically advanced infrastructure (RIS-PACS) supported with interactive multimedia components, advanced visualization, and communications (voice message/text/messenger app-based communication, etc.). All these features help in low TAT, quality reporting, and increase the Physician’s satisfaction and confidence with service resulting in the effective clinical outcome – patient care. In today’s competitive world where the patient is ready to go extra mile for better information, better patient care, better treatment option; Teleradiology empowers the referring physician with that winning edge.
At Cloudex, we support you to have that winning edge.