Dr. Shriram Varadharajan, Consultant Neuroradiologist (Neuroimaging & Stroke)
Awareness of stroke and immediate arrival to the hospital plays a major role in its treatment and recovery. Unlike acute coronary syndrome (ACS – heart attack) where pain plays a prominent role in patients presenting early, stroke patients ignore the negative signs such as sudden onset weakness or numbness. Often minor stroke or TIA (transient ischemic attack) serves as a warning for subsequent major stroke (CVA – cerebrovascular accident). Stroke patients need to complete timely evaluation with various imaging tools. Treatment decisions in acute stroke require ultrafast imaging. It should be performed immediately after clinical triage and emergency stabilization of the patient.

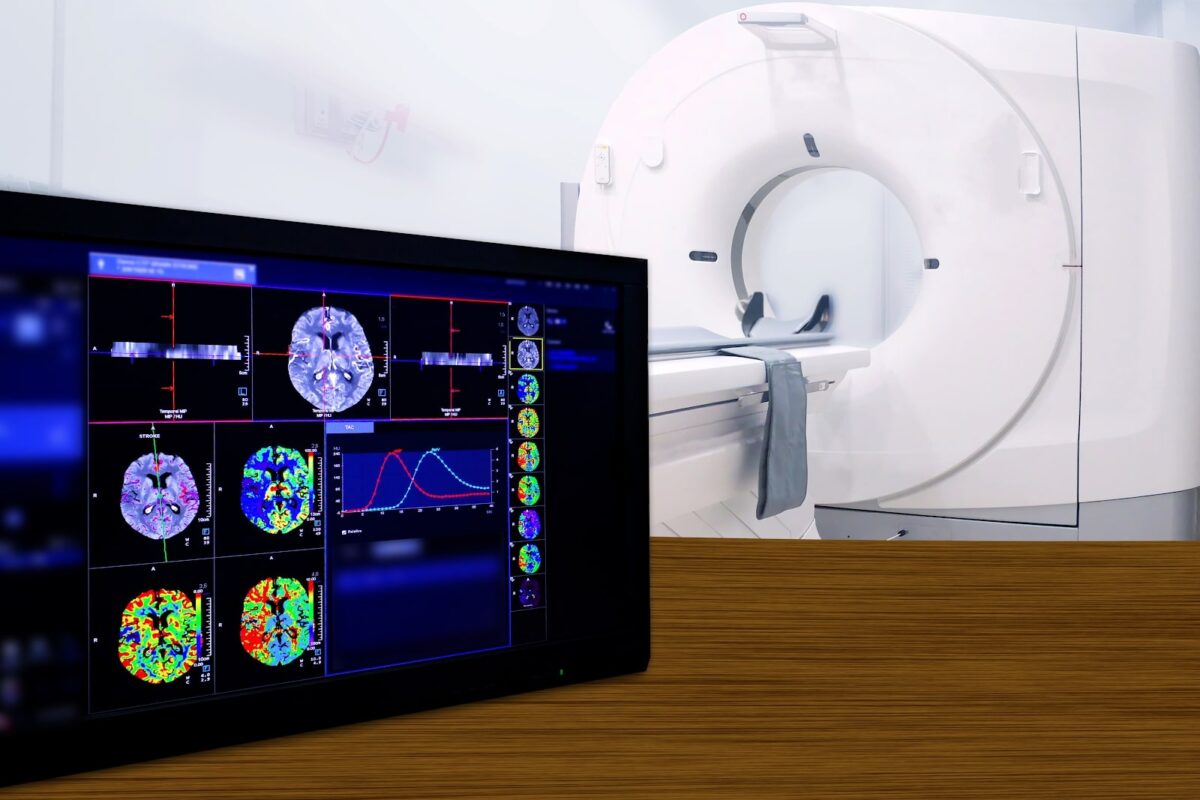
Imaging starts with the very basic question of differentiating Ischemic (clot in the vessels supplying the brain) from Hemorrhagic stroke (bleed) using a simple plain CT scan. Ischemic stroke patients may be given an injection called intravenous thrombolysis (IVT or clot lysis). Plain CT aims to exclude hemorrhage and established large infarcts which are contraindications to intravenous thrombolysis. Additional findings such as hyperdense vessel sign and ASPECTS are helpful to decide on endovascular thrombectomy. Further vascular imaging (imaging of the blood vessels – CT Angiography) is used in Ischemic stroke to detect patients with large vessel occlusion (LVO) i.e. clot inside larger blood vessels. They may need additional emergency endovascular thrombectomy (EVT or clot removal) using advanced catheter-based techniques in DSA (cath.) lab.
These treatments are currently offered to patients presenting within narrow time windows of stroke onset (3-4.5 hours for injection – IVT and 6 hours for cath. lab – EVT). CTA involves evaluating routine angiography and additional venous/delayed phases, regarding the site and presence of LVO as well as to estimate collateral status.
However, few patients who arrive late (beyond 4.5 to 6 hours and till 16-24 hours) can also be treated based on their imaging if we can identify salvageable penumbra (affected brain parenchyma but without permanent damage) using advanced imaging techniques that analyze brain parenchymal perfusion.
All of these decisions can also be taken collectively and more accurately using MRI. Ultrafast Stroke MRI takes less than 20 minutes using limited protocols and involves basic sequences as well as Angiography. MRI in acute stroke can be done without having to administer intravenous contrast and is especially very useful in differentiating from other mimics. Parenchymal and vascular information both can be obtained. MRI involves DWI for infarct core and MRA for LVO while FLAIR mismatch can be used for IVT in stroke patients with unknown time of onset or wake-up strokes. SWI can help detect thrombus/clot burden in RBC rich clots and serve as a penumbral marker by demonstrating vessels with raised oxygen extraction.
Teleradiology can thus be very effective in acute Stroke if reporting can be accelerated to avoid time delays. Simplified reporting formats can be developed based on local logistics. Although CT and CTA are widely practiced in acute stroke, MRI provides a non-contrast one-stop solution in the emergency especially if reported immediately by dedicated, trained tele-stroke Radiologists. Structured reports for such time-based emergency situations like acute stroke help avoid medico-legal consequences especially in the era of evidence-based medicine and helps guide the referring physicians in making treatment decisions.
References
1. Varadharajan S, et al. Computed tomography angiography in acute stroke (revisiting the 4Ps of imaging). Am J Emerg Med. 2016 Feb;34(2):282-7
2. Varadharajan S. ASAP In Stroke Imaging – Need to Simplify and Standardize in Emergency. Accepted for publication in Neurology India