India is going through a grave crisis with a rising number of Covid cases. People are deprived of timely medical care due to an overwhelmed health care system. People are dying in ambulances and waiting areas for want of beds and essential life support. Health care facilities are facing difficulty in triaging the patients and deciding on whom to treat first. RT-PCR and antigen tests are recording high false-negative rates and there is an inordinate delay in getting the test reports too, which is adding to the delay and confusion in care delivery.
It turns out that the majority of casualties are due to viral pneumonia which is resulting in low blood oxygen saturation levels. Timely diagnosis of the lung pathology and grading of its severity can help save the lives of many. Unfortunately, the endless wait for a diagnosis of Covid by RT-PCR / antigen to decide on hospital admission has taken many a life. There are instances where a breathless patient diagnosed with Covid like pneumonia with CT chest given a score of almost 30 percent of lung affected had to wait for her RT PCR result which came negative twice after waiting nearly 48 hours each time around to get admitted in a hospital. Her wait ended when a hospital agreed to admit her to their SARI (Severe Acute Respiratory Illness) ward despite her RT PCR negative status, but unfortunately, it was too late and she succumbed to the savage virus.
There are innumerable similar deaths happening in all the badly hit cities of India. Hospitals are not able to decide whether to admit or not and if admitted, to the Covid care ward or the non-Covid one. A few hospitals thus decided upon setting up a ward for the breathless and named it SARI (Severe Acute Respiratory Illness) ward like in the case mentioned above. Still, there was a confusion on admission criteria when the Union Health Ministry in its revised national policy for admission of COVID-19 patients on 8th May said “A suspect case shall be admitted to the suspect ward of COVID Care Centre (CCC), Dedicated COVID Health Centre (DCHC) of Dedicated COVID Hospital (DHC) as the case may be,” in the directive to all the states and Union Territories and that no private or government hospital shall deny admission/care to any patient and that positive coronavirus disease (Covid-19) report is no more mandatory for admissions.
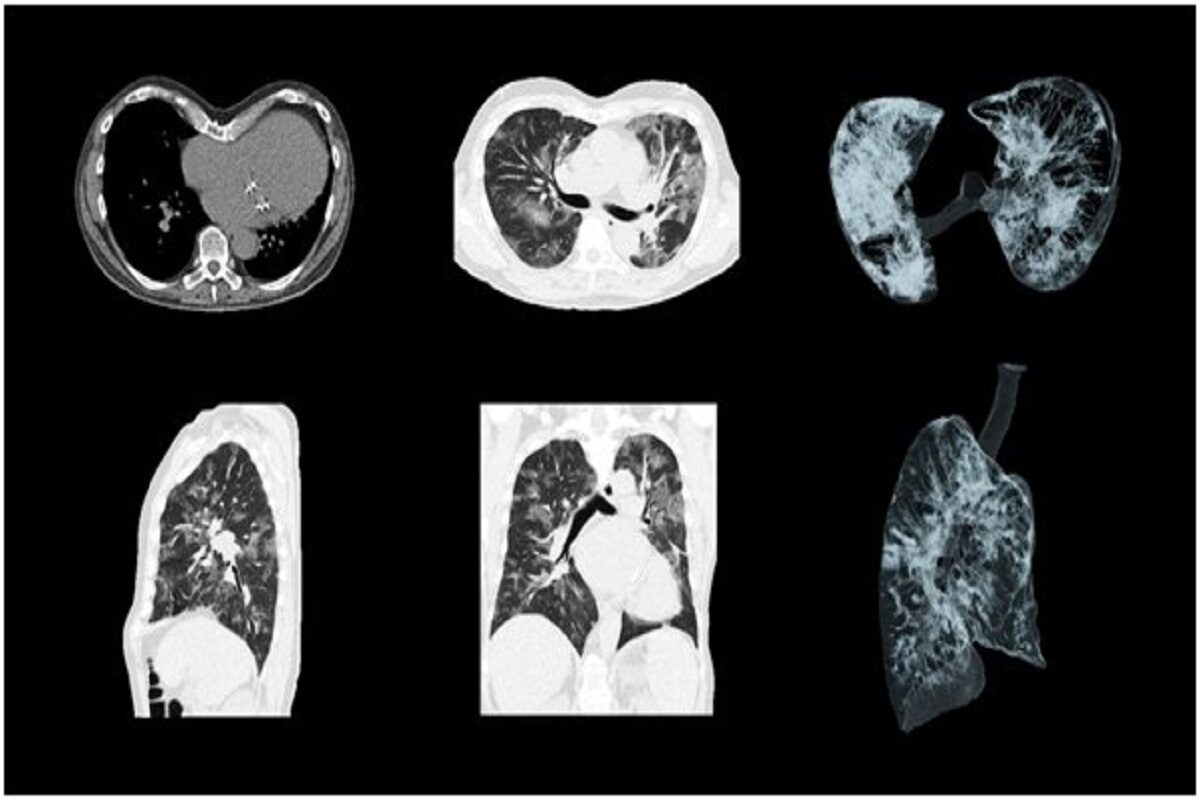
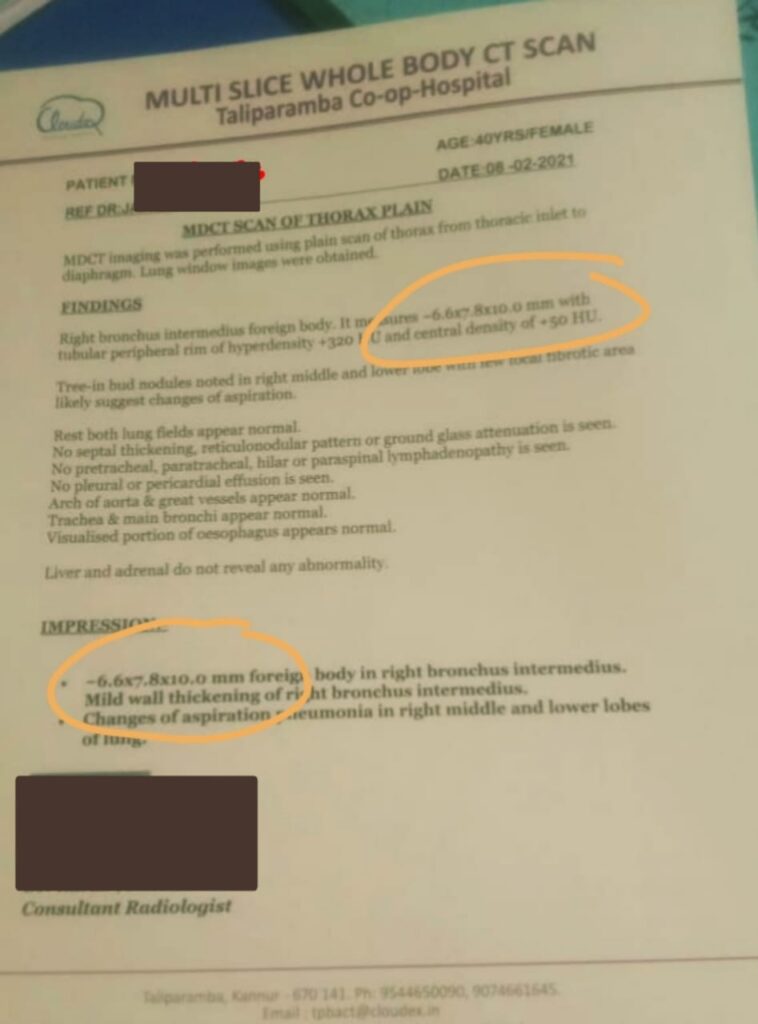
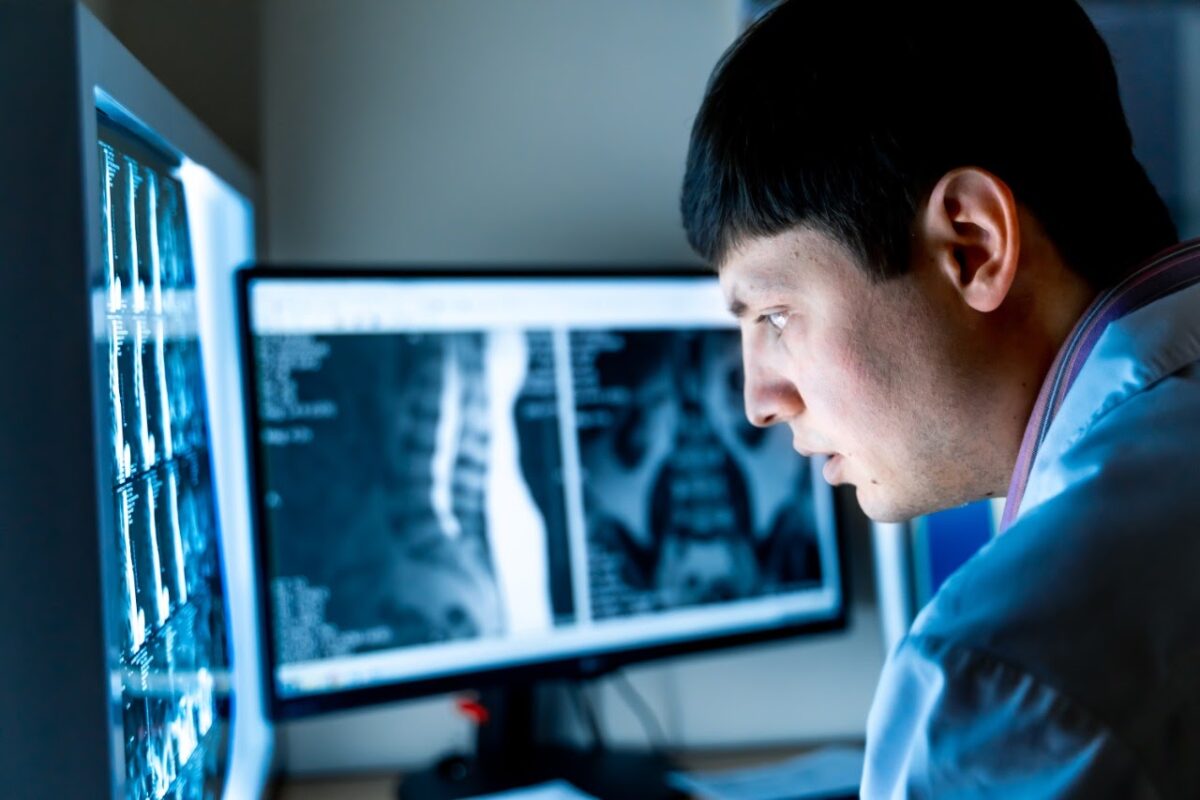
The relevance of a CT chest cannot be emphasized more in the current situation. A CT Chest in the symptomatic patient can quickly assess the lungs and with the help of CORADS score can determine whether the lung is affected or not and classify the disease into non-Covid / low/high possibility of Covid pneumonia. A CT Severity Score of 0-25 out of 25 in the meanwhile can grade the lung involvement into mild (<30%), moderate (30 – 60%), and severe (>60%) disease. The radiologist can quickly assess the CT chest according to these criteria and issue a report, and the quantitative report greatly aids the treating physician to triage the patients and prioritize admission and treatment delivery.
In the current pandemic scenario, the Turn-around-time (TAT) of any diagnostic test (imaging, laboratory, or pathological) plays a crucial role in diagnosis and saving a life. The highly virulent strain of COVID is playing its trick with widely conducted RT-PCR but gets caught in CT Chest. While RT-PCR results are taking up to 48-72 hours at many places due to the unmanageable load, CT chest reports are delivered in less than an hour and are helping physicians in faster diagnosis, prioritization of admissions, and treatment plan for the sick and high-risk patients with comorbidities.
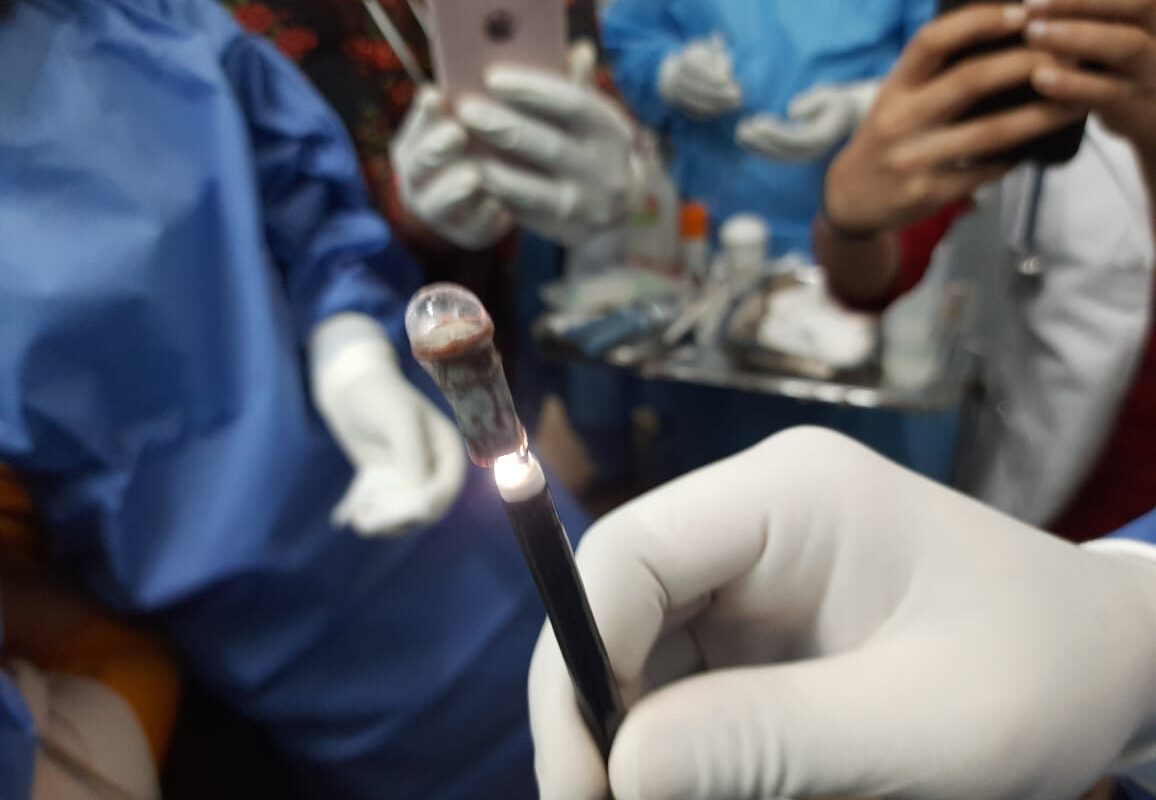
The Healthcare system is facing multifaceted challenges, the biggest one being the shortage of staff and expertise. Hospitals and diagnostic centers are looking for support in a quick, accurate diagnostic process with an unmanageable number of cases every hour. Teleradiology is capable of providing the required support in reporting the large numbers in less time irrespective of the system’s location (urban/rural). Simultaneously serving multiple centers, each teleradiology system has its own team of radiologists and TAT management protocols wherein reports are delivered in promised time despite the large volume.
The teleradiology service providing consistency, shorter TAT, and quality reports benefit the referring physician- aids in diagnosis and guides treatment plan; develops a strong relationship with its client resulting in delivery of quality patient care with high patient satisfaction score.
We at Cloudex have absorbed the gravity of the situation and are working 24*7*365 doing our best to help and serve the country’s healthcare system in this crisis. Our promise to the needy is a report within 30-45 mins for every suspected Covid CT Chest.
Cloudex Radiology Solutions delivers shorter TAT than agreed upon … benefiting referring Physician’s quick action.
Cloudex’s team including administration, operation, and teleradiologists are encouraged to develop a close relationship with the client’s team for familiarity and communication comfort; resulting in delivery of reports within TAT bundled with quality and accuracy. Here, strategically knitted workflow incorporated with advanced technology and expertise ensures the shortest TAT without compromising on the quality that serves & impresses the clients.
The team also emphasizes performance measures, report quality, communication with the referring physician apart from TAT which contributes to the partnered client’s undivided focus on patient care delivery. These efforts of both teams help in remaining competitive and having a winning edge in demonstrating value-based service delivery.
At Cloudex, we support you to have that winning edge.